Dark spot/brown spot –
WHAT IS IT
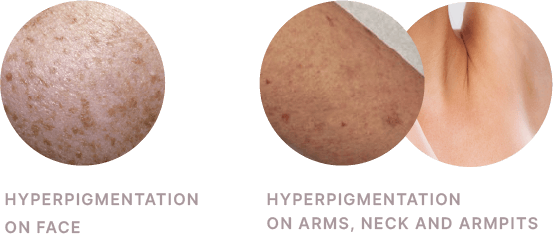
Dark Spot are hyperpigmentation on face and body, which are the result of excess melanin production, distribution, or transport.
Melanin is a term referring to a group of dark-brown to black pigments produced from the oxidation of amino acid tyrosine, followed by polymerization.
This process is happening in the melanocyte, a type of cells located in the basal layer of the epidermis, with dendrites that extend into more superficial layers of the epidermis.
The melanin produced inside of the melanocyte is packaged into a melanosome (“sack” of pigment), and then transferred into the keratinocyte.
The keratinocytes migrate to the stratum corneum where visible pigment clusters are formed.
MOST COMMON HYPERPIGMENTATIONS


please access the session indicated for you:
Dark spot/brown spot –
WHAT IS IT
Follow the most common hyperpigmentations observed in current practice.
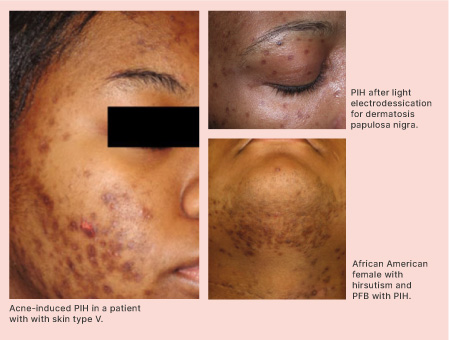
1. Dark spot/brown spot (Post inflammatory hyperpigmentation):
PIH is an acquired hypermelanosis occurring after cutaneous inflammation or injury that can arise in all skin types, but more frequently affects skin-of-colour patients, including African Americans, Hispanics/Latinos, Asians, Native Americans, Pacific Islanders, and those of Middle Eastern descent [88].
PIH results from the overproduction of melanin or an irregular dispersion of pigment after cutaneous inflammation.
When PIH is confined to the epidermis, there is an increase in the production and transfer of melanin to surrounding keratinocytes.
2. Solar lentigines (Liver spots):
They are macular, 1- to 3-cm, hyperpigmented, wellcircumscribed lesions on sun exposed surfaces of the skin.
They vary from light yellow to dark brown and often have a variegated appearance. These hyperpigmented spots are also known as lentigines, age spots, and liver spots.
3. Ephelides (Freckles):
Freckles are small, 1- to 2-mm, sharply defined macular lesions of uniform colour, most often found on the face, neck, chest, arms, and legs.
Colour may vary from red to tan to light brown, and number from a few to hundreds. Onset is usually in childhood after sun exposure.
4. Café au lait macules
About 10% to 30% of the general population has an isolated café au lait macule. They are asymptomatic and do not require treatment. They result from an increase in melanin concentration in melanocytes and basal keratinocytes.

Current treatment of hyperpigmentation
In order to be effective, the hyperpigmentation therapy should be:
1. Multi-modal: Monotherapy is not enough. Typical treatment consists of a combination of the following:
– Procedures.
– Prescriptions.
– Cosmeceuticals.
2. Multi-step: Topicals and procedures are used in multiple treatments over time:
– Prime skin with regimen of cosmeceuticals and/or prescriptions.
– Perform clinical procedures like lasers or peels.
– Cosmeceutical and/or prescription regimen continues.
– Additional clinical procedures.
3. Multi-layer:
– Exfoliate existing pigment at skin’s surface.
– Inhibit melanin transfer.
– Block excess melanin production at basal layer.
– Deactivate inflammatory mediators and decrease melanocyte activity.
Procedures
Lasers and light therapies
LASERS
• Green (510nm, 532nm), red (694nm), or near-infrared (755nm, 1064nm) lasers are pigment-specific and generate light used to selectively target intracellular melanosomes.
• Energy from short wavelength lasers is more efficiently absorbed by epidermal melanin while longer wavelengths penetrate deeper with more selective absorption by dermal targets.
• The use of longer pulse durations and cooling devices can also provide a greater margin of safety while still maintaining efficacy.
Chemical Peels
Glycolic acid (GA): found in sugarcane, is a naturally occurring alpha-hydroxy acid (AHA) that induces epidermolysis, disperses basal layer melanin, and increases dermal collagen synthesis [161]. GA concentrations range from 20 to 70%, and neutralization with water or sodium bicarbonate is required to terminate the peel.
Salicylic acid (SA): derived from willow tree bark, is a beta-hydroxy acid that induces keratolysis by disrupting intercellular lipid linkages between epithelioid cells [96]. Superficial SA peels utilize concentrations ranging from 20 to 30% without the need for neutralization.
Superficial chemical peels: can also be obtained using trichloroacetic acid (TCA) or Jessner’s solution, and both agents have been efficacious in the treatment of Melasma [164.165]. Most superficial chemical peeling agents are well tolerated by Fitzpatrick skin types IV to VI. Common side effects include erythema, burning sensation, PIH, reactivation of HSV, superficial desquamation, and vesiculation.

Prescription Therapies
Hydroquinone: Prescribed in concentrations from 2 to 12%.
Tyrosinase inhibitor.
Tretinoin: Retinoic Acid in concentrations from 0.025- 0.1%.
Strong rejuvenating and keratolytic agent to remove pigment clusters and stimulate cell renewal.
*Note: Pure Retinol cosmeceuticals in concentrations above 0.3% are a well-tolerated alternative to Tretinoin.
Azelaic Acid: Prescribed in 15% concentration Anti-inflammatory, Tyrosinase inhibitor. Less common than Hydroquinone

Cosmeceutical Therapies I
Common cosmeceuticals provide active ingredients used as alternatives to hydroquinone that are generally tyrosinase inhibitors with action limited to the epidermis.
HYDROQUINONE (HQ):
• Adverse events reported with HQ use include contact dermatitis, nail discoloration, permanent leukoderma, and hypopigmentation of the surrounding normal skin that has been treated with HQ (“halo effect”).
• Patients may also develop exogenous ochronosis (EO), typically associated with frequent use of very high concentrations of HQ on a long-term basis.
MEQUINOL:
• Derivative and alternative to hydroquinone.
• Thought to be less irritating to the skin than HQ.
• Mechanism of action may involve a competitive inhibition of tyrosinase.
KOJIC ACID:
• A fungal metabolite of certain species of Acetobacter, Aspergillus, and Penicillium.
• Works by potent inhibition of tyrosinase by chelating copper at the active site of the enzyme.
• Available in 1 to 4% concentrations and can be formulated with other lightening agents, including glycolic acid and hydroquinone, to increase efficacy.
AZELAIC ACID (AA):
• Naturally occurring as a dicarboxylic acid isolate from the organism responsible for Pityriasis versicolor.
• AA has several mechanisms by which it depigments the skin including tyrosinase inhibition as well as selective cytotoxic and antiproliferative effects toward abnormal melanocytes through the inhibition of DNA synthesis and mitochondrial enzymes.
• Exists in formulas at 15% and 20%.
ARBUTIN:
• Extracted from the dried leaves of the bearberry shrub or pear, cranberry, or blueberry plants.
• Another derivative of HQ, without the melanotoxic effects.
• Causes depigmentation by inhibiting not only tyrosinase activity but also melanosome maturation.
• High concentrations of arbutin can lead to a paradoxical hyperpigmentation.
VITAMIN C:
• A naturally occurring antioxidant obtained from certain fruits and vegetables.
• Causes skin lightening by interacting with copper ions at the tyrosinase active site and by reducing oxidized dopaquinone.
• Antioxidant effects, but some also anti-inflammatory and photoprotective properties.
• Typically used in 5 to 10% concentrations, with special care regarding stability.
Common cosmeceuticals provide active ingredients used as alternatives to hydroquinone that are generally TYROSINASE GLYCOSILATION INHIBITORS with action limited to the epidermis.
N-ACETYL GLUSOSAMINE (NAG):
• An amino sugar precursor to hyaluronic acid and found throughout nature and human tissues.
• Acts by inhibition of tyrosinase glycosylation, a step necessary in the production of melanin.
• NAG-containing cosmeceuticals show greater stability, better skin penetration, and overall tolerability than glucosamine-containing ones.
• NAG is typically used in 2% concentrations as monotherapy or in combination with niacinamide.

Cosmeceutical Therapies II
Common cosmeceuticals provide active ingredients used as alternatives to hydroquinone that are generally WORKING ON MELANOSOME TRANSFER with action limited to the epidermis
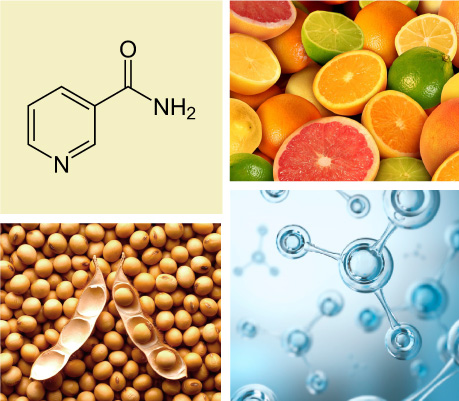
NIACINAMIDE (or NICOTINAMIDE or VITAMIN B3):
• The physiologically active derivative of vitamin B3 or niacin.
• Decreases melanosome transfer to keratinocytes without inhibiting tyrosinase activity or cell proliferation.
• May also interfere with the cell-signalling pathway between keratinocytes and melanocytes to decrease melanogenesis.
• Concentrations of use range between 2% and 5%.
PAR-2 INHIBITORS:
• The activation of protease-activated receptor 2 (PAR-2) cell receptors found on keratinocytes mediates the transfer of melanosomes from melanocytes to keratinocytes.
• Soy proteins inhibit the activation of these cell receptors, and as a result, phagocytosis of melanosomes into keratinocytes is reduced leading to reversible depigmentation.
• Now formulated alone or in combination with other agents including retinol and sunscreen.
Common cosmeceuticals provide active ingredients used as alternatives to hydroquinone that are generally TYROSINASE DOWNREGULATORS with action limited to the epidermis.
RETINOIDS:
• Structural and functional analogues of vitamin A.
• Exert modulation of cell proliferation, differentiation, and cohesiveness; induction of apoptosis.
• Concentrations range from 0.01 to 0.1% and tretinoin can be formulated in creams, gels, and microsphere gels.
• Third-generation retinoids, adapalene and tazarotene, are synthetic topical agents that are also effective in the treatment of hyperpigmentations.

















DO YOU KNOW?
Air pollution is the primary cause to the hyperpigmentation skin
Whenever a prolonged and repetitive exposure to environmental stressors exceeds the skin’s normal defensive potential, there is a disturbance in the skin barrier function leading to the development of skin hyperpigmentation.
Source: Current environmental health reports
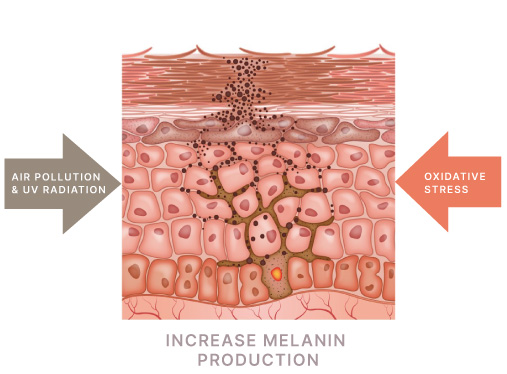
In UV Radiation and Traffic-Related Air Pollution where huge amount of free radicals set ready to attack healthy skin cells
Tropospheric ozone (O3)
O3 is formed in a chain of complex photochemical reactions, requiring the presence of nitrogen oxides, volatile organic compounds, other air pollutants, and solar radiation.
O3 was shown to rapidly oxidize the macromolecules in the skin, such as lipids and proteins, producing radical species, such as hydroxyl radical, and triggering oxidative stress *.
* Krutmann J, Liu W, Li L, Pan X, Crawford M, Sore G, et al. Pollution and skin : from epidemiological and mechanistic studies to clinical implications. J Dermatol Sci. 2014;76:163–8. 38. Valacchi G, Lim Y, Belmonte G, Miracco C, Zanardi I, Bocci V, et al. Ozonated sesame oil enhances cutaneous wound healing in SKH1 mice. Wound Repair Regen. 2011;19:107–15

AIR POLLUTION & HYPERPIGMENTATION
Interaction between Air Pollution and UV Radiation
Under physiologic conditions and in urban environments, human skin is exposed to both solar UVA/UVB radiation and traffic-related air pollution.
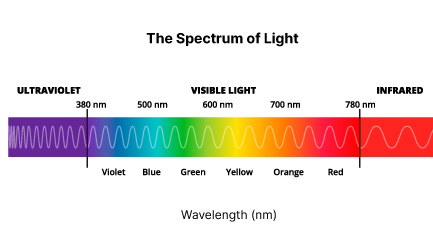
UV radiation comprises UVC (100–280 nm), UVB (280–315 nm), and UVA (315–400 nm).
UVA and UVB can penetrate the atmospheric ozone layer → detrimental effects on the skin (photoaging and uneven skin pigmentation).
UVB radiation is the most energetic → penetrates the superficial skin layers down to the epidermal basal layer.
UVA is less energetic (present in larger amounts) → penetrates deeper into the skin reaching the dermis.
An interplay between UV and PM* → cause facial lentigines.
A negative interaction between PM and UV on pigment spot formation: At higher PM levels, associations with UVB became weaker and, vice versa, at higher UVB levels, associations with PM became weaker.

RECOMMENDATION:
Regimen to enhance efficacy in hyperpigmentation treatment
LSI’s investigators introduce a 3-step routine to boost the effectiveness of hyperpigmentation management:
PREVENT – CORRECT – PROTECT, 3 actions to fight hyperpigmentation.
The recommendation includes a day and night routine with the use of different natural active ingredients acting at different levels of the skin.
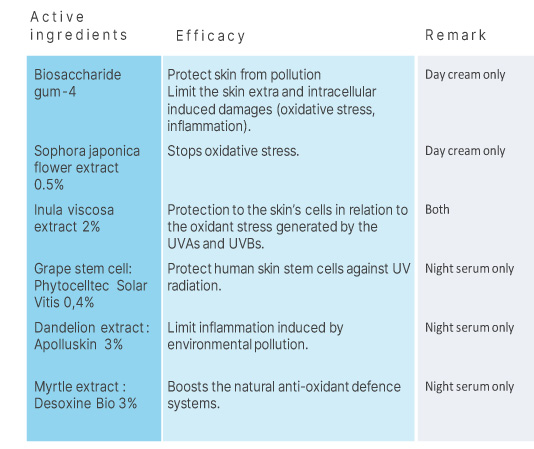
STEP 1 – Prevent
ESSENTIAL STEP: PREVENT FUTURE SKIN DAMAGES CAUSED BY ENVIRONMENTAL POLLUTION THAT RELENTLESSLY HAPPEN
BIOTOPIX® POLLUSTOP® ANTI-POLLUTION
DAY CREAM & NIGHT SERUM

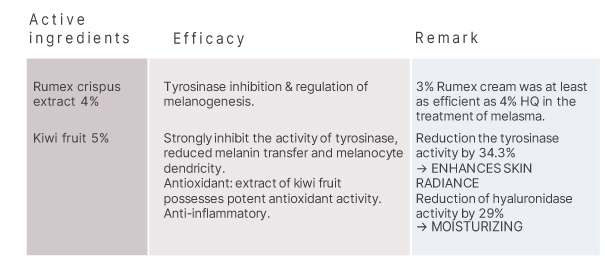
STEP 2 – Correct
CORRECT HYPERPIGMENTATION – MANAGE DARK SPOTS/BROWN SPOTS
AMELIX® BROWN SPOTS
FACE CREAM & BODY EMULSION

STEP 3 – Protect
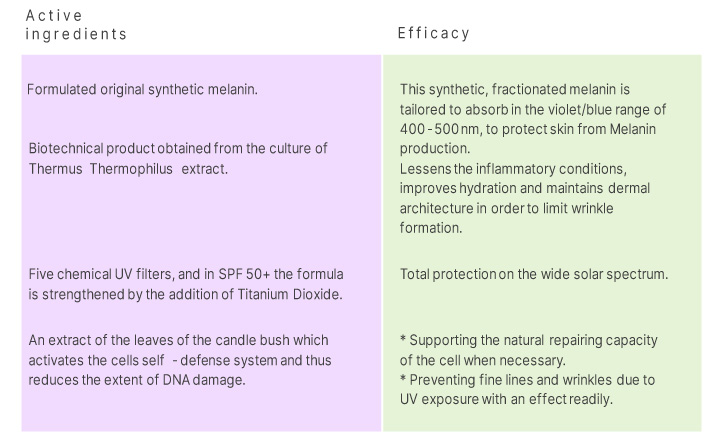
PROTECT THE SKIN USING FULL-SPECTRUM PHOTOPROTECTION, ESPECIALLY AS REGARDS THE DAMAGE CAUSED TO THE SKIN NOT ONLY BY UVR, BUT ALSO BY VISIBLE LIGHT AND IR RADIATION
BIOTOPIX® PHOTO PROTECT®
SPF30 or SPF50+

HOW TO USE: PREVENT – CORRECT – PROTECT
Morning & Night routine
In the morning
1: Cleansing & toner.
2: Apply a small amount of AMELIX® Brown Spots Face Cream and Body Emulsion on the dark spot areas only → gently massage to make it penetrate.
3: Apply BIOTOPIX® POLLUSTOP Anti-Pollution Day Cream on full face → gently massage to absorb it well.
4: Make up is possible after complete penetration.
5: Protect Skin with BIOTOPIX® PHOTO PROTECT SPF30 or SPF50+ depends on how strong sunlight exposure.

At night
1: Cleansing & toner.
2: Apply BIOTOPIX® POLLUSTOP Anti-Pollution Regenerative Night Serum on full face → gently massage to make it penetrate.
3: Apply AMELIX® Brown Spots Face Cream and Body Emulsion on the dark spot areas only → gently massage to make it penetrate.